June 27th, 2024
Anesthesia Employment Models for Hospitals and Healthcare Systems
Written by Howard Greenfield, MD, Principal, and Robert Stiefel, MD, Principal – Enhance Healthcare Consulting
We have recently seen a dramatic increase in hospitals choosing to transition to employment of their anesthesia providers. In this article we will explain the drivers behind this trend and discuss key items for consideration when contemplating employment of anesthesia providers.
Anesthesia groups have traditionally been independent, often with an exclusive contract with a hospital or health system. Since the early 2000s the frequency and magnitude of hospitals requiring financial support to secure anesthesia services has continued to climb, with over 90% now paying stipends to secure anesthesia coverage. As stipend amounts continue to escalate exponentially into the millions and sometimes tens of millions of dollars, many hospitals view this level of financial support as de facto employment. In response, many hospitals and health systems have come to believe that the employment of their anesthesia service offers the clearest path to control spending and maximize coordination of care.
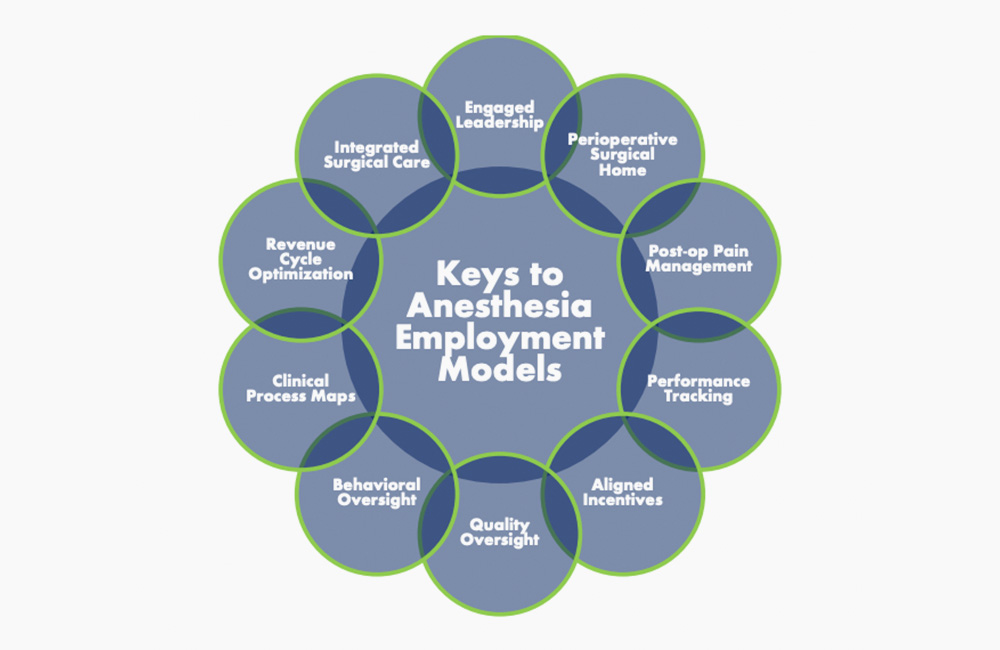
As new anesthesia employment models are created and existing arrangements restructured, facilities will be best served by creating a framework to align anesthesia providers, OR nurses, surgeons, and proceduralists as true partners. The most successful models will facilitate integration while incentivizing OR efficiency, customer service, and optimizing patient care. Having supported several anesthesia employment arrangements in the last few years, we developed the top 10 areas hospitals should focus on when considering transition.
Engaged Leadership
Identifying the best incumbent leaders or seeking experienced anesthesia leadership outside the organization to create a supportive group culture is crucial for success. Successful anesthesia leaders must communicate continuously with surgeons, operating room staff, and hospital leadership. They should strive to improve the quality, safety, and efficiency of surgical care and be actively involved in tracking performance and outcomes. Anesthesia directors are expected to participate in all perioperative committees and play a key role in OR process improvement initiatives.
Perioperative Surgical Home (PSH)
Prevailing reimbursement mechanisms lead many anesthesia groups to focus resources on intraoperative care. To optimize the anesthesia value proposition in an integrated delivery system, expectations for services should expand to encompass the concept of the PSH, addressing the entire perioperative continuum – from patient preoperative preparation to postoperative discharge and recovery. Successful models position the anesthesia provider group as a leader with surgeons and OR nursing support to ensure a consistent and data-driven approach to the perioperative experience. Protocols for evidence-based practice and postoperative pain management should be established, and the anesthesia group should be positioned to incorporate them into the PSH methodology.
Post-Operative Pain Management
The use of indwelling catheters, long-acting regional blocks, and new intraoperative medications can significantly reduce postoperative pain. Anesthesia groups adopting such techniques can improve patient satisfaction scores and reduce postoperative complications and length of stay. Ensuring that your group incorporates a culture that supports post-operative pain management can be a competitive advantage and help support surgeon satisfaction and procedural growth.
Performance Tracking
Metrics related to the quality and efficiency of anesthesia services should be measured and linked to a portion of provider compensation. Obvious items include MIPS measures like sterile technique during central line placement and maintaining normothermia. Metrics specific to each organization’s goals should also be included, such as surgeon satisfaction scores, day-of-surgery cancellations due to anesthesia, completion of preoperative evaluations prior to the day of surgery, and labor and delivery response time. Displaying important metrics monthly as a departmental scorecard or KPI dashboard tracked by facility and group leaders is beneficial.
Aligned Incentives
While productivity and performance incentives are commonly included in physician employment agreements, the calculations for anesthesia groups are somewhat unique. Providers typically receive base compensation, but increasingly, components of compensation are placed at risk based on several anesthesia efficiency and compliance measures such as FCOTs, narcotic reconciliation, support of OR utilization, performance, and quality.
Quality Oversight
As reimbursement becomes increasingly linked to quality and outcomes, anesthesia departments must track and document anesthesia-specific clinical quality metrics for individual providers as well as the entire department. These measures should be benchmarked, tracked, and trended regularly.
Behavioral Oversight
Inappropriate behavior by anesthesia providers can negatively impact group culture, OR staff morale, and surgeon satisfaction. Many groups are unwilling or unable to monitor or address inappropriate behavior. Predefined mechanisms for tracking and evaluating behavioral issues through peer review, and identifying the consequences of such actions, should be in place for all hospital-based physician groups.
Clinical Process Maps
Inconsistencies in anesthesia providers’ responses to common clinical issues are a frequent source of dissatisfaction among surgeons and OR staff. Variations may include lab value abnormalities, preoperative preparation of patients with cardiac disease, NPO status, and requirements for consultation reports. Consistency leads to customer satisfaction. A hospital employment model gives the OR governance committee and anesthesia group leaders an ideal opportunity to develop and enforce written policies to address variations in common clinical practices.
Revenue Cycle Optimization
RCM management requires expertise in time-based billing, provider documentation, concurrency, and compliance. Most hospitals do not have this internal capability and are best served by outsourcing revenue cycle functions to well-established, anesthesia-specific firms to ensure compliant billing, optimization of professional collections, and development of accurate, actionable reporting. An outsourced revenue cycle firm can also manage commercial payer contract negotiations to optimize performance.
Integrated Surgical Care
One clear theme in healthcare optimization efforts is the need for closer integration throughout the continuum of care. In the OR, this involves closer clinical and process-related coordination among anesthesia providers, surgeons, proceduralists, OR nurses, and other supporting services. An employed anesthesia provider should be at the forefront, creating a tightly aligned delivery model for all surgical cases throughout the entire hospital or health system.
Summary
Facility leaders should recognize that applying a “cookie-cutter” approach designed for primary care and referring specialists to employment of anesthesia providers is not a blueprint for success. The keys discussed above offer a framework to create an optimally aligned model, incorporating the unique attributes of anesthesia practice, as well as the boundaries and limitations within which anesthesia can have a positive impact on your surgical services. Working with anesthesia subject matter experts to support the transition, optimize revenue cycle performance, and co-manage employed models will ensure that your newly employed practice is positioned for surgical volume gains in today’s market while creating an important foundation to optimize the delivery of surgical care.
Learn more about Enhance Healthcare’s Anesthesia Employment Transition Assistance.
Email: info@enhancehc.com
Phone: 954-242-1296
